Eradicating Pseudomonas aeruginosa from drinking water installations
Pseudomonas aeruginosa poses a serious risk to human health, and especially in places that are frequented by vulnerable groups of people such as healthcare facilities and day nurseries. In hospitals, this bacterium is the second most common pathogen for pneumonia, the third most common for urinary tract infections and the eighth most common for blood poisoning. Read on for tips on how best to avoid contamination with Pseudomonas aeruginosa in the first place – and effective strategies for remediation in a worst-case scenario.
Pseudomonas aeruginosa in healthcare facilities
Unless drinking water is being bottled, Pseudomonas aeruginosa is not a parameter included in the routine analysis of drinking water according to German law. This is because Pseudomonas aeruginosa does not pose a threat to the general population. Since 2006, however, a recommendation from the Federal Environmental Agency, following a consultation with the Drinking Water Commission, has stipulated testing for this parameter in hospitals as well as other (health)care facilities. This recommendation was updated in 2017.
The German Society for Hospital Hygiene (DGKH) – most especially in the person of its President, Professor Martin Exner – has repeatedly made efforts to draw attention to the significance of Pseudomonas aeruginosa as a waterborne pathogen, especially in the case of hospital-acquired (‘nosocomial’) infections. In these facilities, Pseudomonas aeruginosa is the second most common pathogen for pneumonia, the third most common for urinary tract infections and the eighth most common for blood poisoning: it causes around 7,500 deaths annually and therefore significantly more than the already high figure of 3,000 for Legionella.
How does the Pseudomonas aeruginosa bacterium spread?
Pseudomonas aeruginosa has very few requirements for nutrients, which means the bacterium can easily colonise even surfaces on parts fresh out of the factory. It does need water to do so, however. The pathogen also forms biofilms very easily: this affords it excellent protection against drying out, the human immune system and chemical disinfectants. Even if chemical disinfection is used, Pseudomonas aeruginosa can still be found in waste traps, soaps and descaling systems. The bacterium also reproduces extremely quickly: its colony count doubles after just 20 minutes, while Legionella needs 2 to 4 hours to achieve this. The pathogen can also move around and even grow around seals. This explains how drinking water installations can also become contaminated via rarely used tapping points – and therefore against the flow of water. Unlike Legionella, Pseudomonas aeruginosa is also facultatively anaerobic (can do without oxygen).
Eradication strategies and approval audits
Pseudomonas aeruginosa has one key weakness: the pathogen is significantly more sensitive to temperature than Legionella and is killed off at temperatures as low as 45 °C. By way of comparison, Legionella needs to be kept at 70 °C for 3 minutes to be killed off – this rises to 30 minutes at 60 °C. Accordingly, Pseudomonas aeruginosa is typically a bacterium found in potable water cold (PWC), as long as potable water hot (PWH) is always 45 °C and over. However, PWH can also become critical if temperatures drop below this level, which is true of many mini tankless water heaters. Furthermore, the bacterium is also surprisingly non-competitive, which means it has difficulty establishing itself in older installations.
In light of the above, it is understandable that eradication efforts usually opt for thermal disinfection in combination with ensuring the proper maintenance of specified normal operation.
Chemical disinfection is a less expedient strategy, as Pseudomonas aeruginosa can retreat into its biofilm. Even our immune systems have trouble tackling it there. The pathogen also likes to colonise seals, which are largely bypassed by the flows of liquid chemical disinfectants. The reverse is true for high temperatures, however: these penetrate every biofilm and any gap in the drinking water installation, no matter how small, not least as a result of the thermal conductivity of the materials.
A new ward block located in Germany’s Middle Rhein region had to have its drinking water installation fully dismantled even before commissioning, because chemical disinfection had not achieved the desired results. Although the bacteria in the installation’s water had been safely killed off, this was not necessarily the case on its surfaces – and biofilms. This explains why contamination is often found again after completing chemical disinfection. The chemical disinfection system has to be switched off after each eradication attempt, and if it has not dispatched all the bacteria in the biofilms, then these can simply re-contaminate the water in the system from these surfaces.
This is why DVGW W 551-2 also stipulates three ‘approval audits’ after any type of decontamination: after two, six and twelve weeks.
Remediation work is considered successful only after twelve weeks have passed – and not a day sooner. This fact has to be kept in mind.
In contrast to other forms of microbiological clean-up work, the contaminated part also typically needs to be identified and decontaminated or replaced. Nor is ensuring the full thermal disinfection of a cold water installation particularly straightforward. Logically, all of its components need to be checked for compatibility with such high temperatures – they were designed for use with cold water, after all.
Ultimately, the strategy has to be a thermal disinfection combined with an increased exchange of water across all tapping points. A much more systematic approach is also required compared to decontamination work involving Legionella, as the Pseudomonas bacterium reproduces extremely rapidly. In particular, the fact we are working with PWC means we cannot rely on high temperatures after eradication is complete. In other words: after decontamination work involving Legionella, the hot water line continues to be operated at hygienically safe temperatures (60° C/55 °C), which continue to ‘disinfect’ the system after the actual thermal disinfection. However, we do not have this kind of protection after thermal disinfection of PWC for Pseudomonas aeruginosa. If we have not managed to truly eradicate it, this cold-water bacterium will just start reproducing again.
Summary
Fortunately, we can avoid Pseudomonas aeruginosa contamination by using hygienically safe products, good working practice and ensuring specified normal operation immediately after filling the drinking water installation. And if a case of contamination does happen, an attempt should be made to identify experts who have successfully eradicated this pathogen from multiple installations. Trial and error simply takes too long and becomes prohibitively expensive.
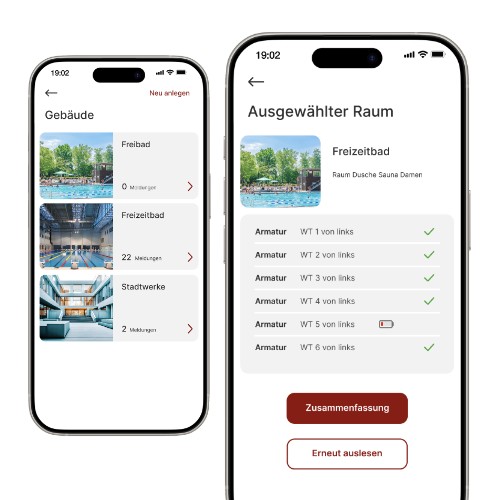
SCHELL SWS Water Management System
To keep Pseudomonas aeruginosa out of an installation, a regular exchange of water across all tapping points is needed. With the SCHELL SWS Water Management System, this specified normal operation can be simulated across all tapping points. If eradication work becomes necessary, SWS can be used for the optimised planning and execution of thermal disinfections.

![[Translate to English:] [Translate to English:]](/fileadmin/_processed_/1/b/csm_symstemloesungen_e2_thumb_6bca267f26.jpg)





















![[Translate to English:] [Translate to English:]](/fileadmin/user_upload/images/menu/menu_service_downloads_broschueren.jpg)








![[Translate to English:] [Translate to English:]](/fileadmin/_processed_/7/7/csm_menu_unternehmen_ueber-schell_awards_f6cec25b1d.jpg)
![[Translate to English:] [Translate to English:]](/fileadmin/_processed_/a/0/csm_menu_unternehmen_ueber-schell_wasser-sparen_41036d2dd9.jpg)